- Home
- The Community News
- Maricopa County Preparing To Expand Contact Tracing
Maricopa County Preparing To Expand Contact Tracing
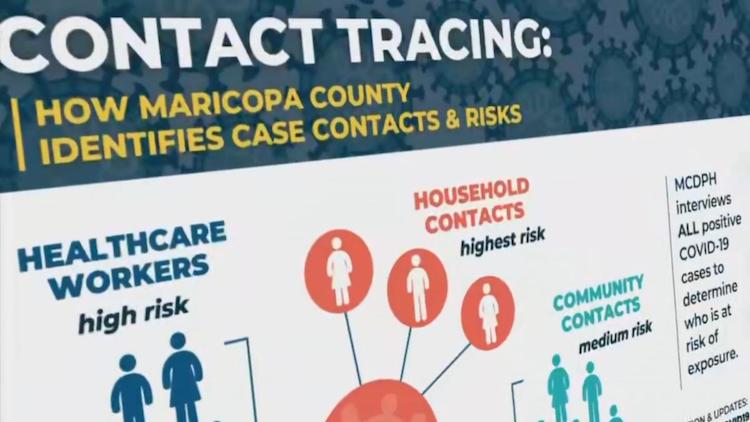
Maricopa County Department of Public Health is preparing to increase its capacity to contact people who have been exposed to COVID-19. In order to best monitor COVID-19 cases and community risk, MCDPH is currently working to implement a plan to scale up its contact tracing capacity by eight to 10 times its current level. MCDPH has done contact tracing for every confirmed case of COVID-19, beginning with Maricopa County’s first case in late January, and this expanded team of contact tracers will help meet the need as more individuals are tested, which will inevitably raise the number of positive cases requiring contact tracing.
“The unified command leadership team at Maricopa County understands that in order to safely lift physical distancing restrictions, there must be certain resources available. Testing, personal protective equipment (PPE) and a comprehensive contact tracing system are a few of those important resources,” said Marcy Flanagan, director of Maricopa County Department of Public Health.
The ability of contact tracing to be as effective as possible relies heavily on the public trust of information shared between community members and public health. Maricopa County places the protection of this information as a top priority and takes every precaution in keeping this information private.
What is Contact Tracing?
Contact tracing has been a fundamental public health practice for over a century and is an important tool in interrupting the spread of infectious diseases. People are most familiar with contact tracing for sexually transmitted disease, tuberculosis and measles.
Contact tracing is conducted by trained investigators who are challenged to be part public health, part detective and part social worker. They must work closely and quickly with positive cases to establish trust, uncover as much information as possible, and then decipher this information to put it into public health interventions.
How Contact Tracing Works
After Public Health receives notice of a positive case from electronic lab reporting, the following occurs:
1. The investigator reaches out to the positive case by phoneand conducts an interview, which can often take hours. They ask a series of questions to gather as much information as they can about who the individual may have exposed while infectious. At the same time, investigators ensure that the individual has all the information they need to know how to best take care of themselves and protect those they love. Questions might include:
- Who are the people in your household? This is because we know they are at the highest risk of getting exposed and developing COVID-19.
- Did you seek healthcare? This is because Public Health will need to make sure proper PPE was worn and ensure that any exposures in the healthcare setting are known.
- Who were you in contact with while infectious? Were you at work? Where do you work? This is because the investigator is trying to discover who of the case’s other contacts could be at risk for exposure.
2. The investigator then reaches out to close contacts and household contactsto educate them on risk of exposure, what to do if they experience symptoms, what they need to do to avoid exposing others and if they need to be quarantined. These conversations are confidential and the positive case’s name is not identified in order to maintain confidentiality of the case’s personal health information. If a contact is required to be quarantined, the investigator will help to ensure the contact’s basic needs, including healthcare and food, are met.
3. The investigator reaches out to healthcare institutionsthat treated the exposed case and ensure proper PPE was worn. Public health then works with facilities to notify any individuals that could have been exposed to this individual.
4. The investigator continues to check up on close contacts to see if they have developed symptoms, depending on how high risk the exposure is – anywhere from daily to at the end of the period when they are no longer at risk of developing disease. Anyone who develops symptoms is given instructions on how to seek healthcare safely without exposing others in the doctor’s office or ER waiting room.
Current Contact Tracing Implementation
The process above is traditional public health contact tracing. About a month ago, as cases rapidly increased and the stay-at-home order went into effect, Public Health changed its investigation process to case-mediated contact tracing. This means Public Health still interviewed every positive case, but worked with the case to reach out to contacts and provided them with all the instructions in writing.
Since the beginning of the COVID-19 outbreak, Public Health has doubled the amount of staff that has been doing investigations to about 25. This includes 5 staff members solely focused on supporting long-term care facilities which also includes skilled nursing facilities, nursing homes, group homes, assisted living, ALTCS (Arizona Long-Term Care System) and rehab facilities.
Plan to Expand Contact Tracing
Currently, Public Health is in the midst of developing a plan to scale up its capacity anywhere between 8 to 10 times from where it is today. As more testing and PPE become available, Public Health will be ready to return to traditional contact tracing for every positive case. More information on this plan will be available very soon. Funding made available to Maricopa County through the CARES Act will help make this possible.